Continence—the ability to control when and where we go to the bathroom—is something most of us learn early in life and often take for granted. That is, until something goes wrong. The term incontinence refers to the loss of control.
Bowel incontinence occurs when someone loses control over gas, liquid stool, or solid stool to the point where it causes discomfort or distress. Urinary incontinence is the loss of control over urine. Bowel incontinence signals that something in the body’s control system isn’t functioning properly.
Experiencing bowel incontinence can be deeply upsetting. Many people feel so embarrassed that they don’t talk about it—not even with their spouse or healthcare provider.
It’s common for people to go to great lengths to hide the condition. In doing so, they may avoid favorite activities, feel a loss of freedom, and withdraw from parts of life they once enjoyed. Without speaking up, they may not get the help they need.
If you experience bowel incontinence, here are three important things to know:
- You are not alone – Many people live with this condition.
- You don’t have to “just live with it” – Treatment is available.
- Help is out there – You can find support and ways to manage it.
Causes of incontinence
Incontinence has many potential causes. While it’s not a normal part of aging, age can increase your risk.
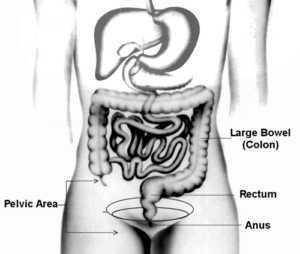
For bowel control to work properly, several systems in the body must function together. If there’s a problem with the pelvic area, incontinence may occur. Injuries, illnesses, physical disabilities, and poor general health are all factors that can also play a role.
The nerves must work correctly to sense when it’s time for a bowel movement or when gas is present. The muscles must then function properly to hold everything in until you’re ready.
Nerve damage caused by conditions like multiple sclerosis, diabetes, or stroke can contribute to incontinence. Injuries from childbirth, surgery, or accidents can also damage the muscles or nerves involved in bowel control.
Common issues such as diarrhea and constipation can also affect continence. These are just a few examples—many conditions that affect men and women can lead to loss of control.
The Effect of Age on Continence
Aside from disease or injury, normal aging can affect continence. As we grow older, our muscles weaken, some nerves lose function, and tissues and organs become less flexible. These natural changes can affect how well the continence system works.
The Bowel Control System
Several things need to happen in your body for you to recognize the need for a bowel movement (or to pass gas) and to hold it in until you’re ready.
The rectum—a tube-shaped organ at the end of the colon—stores stool. As stool moves into the rectum, it stretches to make room. This stretching usually causes the urge to go. Muscles surrounding the rectum tighten to hold stool in until it’s time to release it.
If these muscles are weak, you might feel a sudden, intense urge and may not make it to the toilet in time. If nerves are damaged, you might not even feel the urge, leading to unintentional leakage.
Problems can also occur if the rectum can’t stretch properly or if the muscles don’t respond as they should.
What to do – talking to your healthcare provider
If you experience bowel incontinence, the first thing to do is tell your healthcare provider about it. Most people feel uneasy talking about their stool, intestinal gas, or bowel movements. But providers understand that these are very normal and necessary processes in all of us.
Healthcare providers and other therapists are there to help when bodily processes go wrong. So the first very important step is to talk plainly about the problems you are experiencing.
Begin by describing your troubling symptoms. Be specific so your healthcare provider (or therapist) clearly understands the problem. Here are some examples:
- Diarrhea – Instead of saying “I have diarrhea,” explain, “When I have diarrhea, it leaks into my clothing with little or no warning. I can’t make it to the toilet in time.”
- Constipation – You may be surprised that constipation is another common factor that can lead to incontinence. Hard stool can cause watery stool to leak around it. Make sure to mention both the constipation and the leakage so your provider doesn’t mistakenly treat you for diarrhea.
- Pain – Continually squeezing together the muscles around your rectum, because of fear that stool may leak, can cause the muscles to cramp and get tired. The result will be pain, which can be severe, and muscle weakness. Both will make your incontinence worse. If this is happening to you, explain it to your healthcare provider.
Next, let your healthcare provider know how this is affecting your daily life. Ask yourself this question, “How have my bowel control problems changed my life?” Whether it’s avoiding social events or feeling anxious about leaving home, this information is important for your provider to understand your experience.
These kinds of changes may have come on gradually. They are important for you to recognize. This is your own personal test of how serious your disorder is. How often you experience incontinence is not always as important as how the problem has changed your life. A goal of your treatment will be to help you get back, as much as possible, the parts of your life that have been lost because of incontinence.
If you have lost sensation, you may have no feeling of the urge to pass gas or stool. Knowing you may experience incontinence with no warning, at any time, may mean that you are worried about it all the time. This can be a heavy burden that takes a toll on daily life. Be sure to explain this to your healthcare provider as well.
Your healthcare provider will want to know how long you have been experiencing episodes of incontinence and if it has been getting worse or has changed over time. Other things to tell your provider about include:
Make sure to share:
- How long you’ve had symptoms and whether they’ve changed
- Any other health conditions
- All medications and supplements you take
- Past surgeries
If you are a woman who has given birth, even many years ago, let your healthcare provider know. Tell your them:
- How many children you had by vaginal delivery
- How many hours you were in labor
- If you had an episiotomy (a cut the healthcare provider sometimes makes in the vaginal area)
- If forceps were used
- If you had any tearing that needed surgical repair
Any of these factors could play a part in damage to nerves and muscles, which then get weaker or less able to do their job with age. The resulting problems affecting continence may take 20 or more years to show up.
Your healthcare provider may want to run tests before coming up with a treatment plan. Various tests can look at how well the organs, muscles, and nerves that affect your continence are working. They can also look for signs of disease or injury. The provider should explain to you the reason for the test. You should also understand what to expect during and after the test. If you do not understand something, be sure to ask.
Treating bowel incontinence
The goal of treatment is to improve function, both in your body and in your daily life. Ways to eliminate or reduce symptoms may involve changes in what you eat, bowel retraining, therapy to change the way nerves or muscles respond, surgery, or other therapies.
You can learn strategies that help you manage the symptoms that cannot be cured. Your healthcare provider or therapist can be your partner in putting together an effective treatment and management plan.
Treatment for incontinence involves good communication with your healthcare provider and/or your therapist so you both understand:
- How the disorder is affecting your daily life
- What is the underlying cause
- Factors that bring on an episode of incontinence or makes it worse
Diet
Constipation and diarrhea are common causes that often can be managed. Your healthcare provider or therapist may ask you to keep a diary for a couple of weeks of what you eat and drink. What you do or do not eat and drink can affect how often your bowels move and how hard or loose your stools are.
It is important to learn what foods or drinks affect your bowels so that you can take in more of those that help, and less of those that cause you problems. Your healthcare provider or a registered dietitian can help adjust your diet.
Download IFFGD’s free personal daily diary
Bowel retraining
Bowel retraining works by teaching new skills to develop a regular and predictable schedule for evacuation. This helps decrease unpredictable bowel movements. Healthcare providers, nurses, or therapists who are skilled in treating disorders of the colon or rectum can help you with this. The bowel retraining will include methods, and sometimes medicines, to help normalize stool consistency so the stool is formed (neither too hard nor too soft), and to establish and stimulate a regular time for having a bowel movement.
Read more about bowel training
No matter what the cause of incontinence, dietary and bowel retraining measures can often help. Additional treatment may be needed if nerves or muscles in the pelvic floor area are not working properly.
Biofeedback
Biofeedback is a painless therapy that uses special sensors and a video screen to help improve the nerve sensation and muscle control needed to control bowel movements. Working with a therapist skilled in using biofeedback for disorders of the pelvic floor and rectum can help you improve your ability to sense contents in the rectum and to hold in the contents.
Other treatment options
Other newer procedures are being developed to treat incontinence. These range from electrical stimulation to implants to injections. If the muscle is damaged but the nerves are functioning, surgery is sometimes suggested. Another option some people choose when other treatments fail is to have a colostomy; this involves a surgical procedure to divert stool to a pouch outside the body.
Be sure to talk to your healthcare provider about all options, possible risks, and chances of success. Think about what “success” means to you. Does it mean cure, or does it mean managing symptoms so you can get on with your life? A cure may not be possible. Treatments may have their own set of side effects. It is important that you understand your options and work with your healthcare provider or therapist to set your own treatment goals.
Putting it all together
Incontinence is a symptom – a sign that something is wrong. Treatment may improve, but not always cure the symptom. There are ways to help manage incontinence. The first step is to recognize that something is wrong and seek help.
Unfortunately, many healthcare providers receive little training on bowel incontinence. If your provider doesn’t seem concerned or informed, it’s okay to seek a second opinion. You deserve someone who listens, takes your symptoms seriously, and works with you to find effective solutions.
Adapted from IFFGD Publication: Bowel Incontinence and Aging by William F. Norton, Publications Editor, IFFGD, Milwaukee, WI; and Jeannette Tries, PhD, Director of Therapy Services, Aurora Women’s Pavilion of West Allis Memorial Hospital, WI, and Director of Biofeedback Services, Continence Control Service, University of Illinois, Chicago, IL.
